
kidney transplant guideline 2024
This comprehensive guideline, provides an in-depth exploration of kidney transplants, covering the vital functions of kidneys, the stages of chronic kidney disease (CKD), and the reasons for necessitating a kidney transplant. It delves into the specifics of kidney transplant surgery, including the types of transplants and the process involved. Additionally, the document examines the financial aspects, comparing the costs and notable considerations across different countries. It also addresses life expectancy post-transplant, symptoms and management of kidney rejection, requirements for kidney donation, and the risks associated with kidney donation. Moreover, the review offers insights into the post-transplant recovery process, ethical issues, and the best countries for undergoing a kidney transplant, with a particular focus on Iran's medical tourism. It further discusses the advantages and disadvantages of kidney transplants, legal issues surrounding kidney donation, transplantation in babies, essential post-transplant medications, recovery timelines, and the waiting list for transplants.
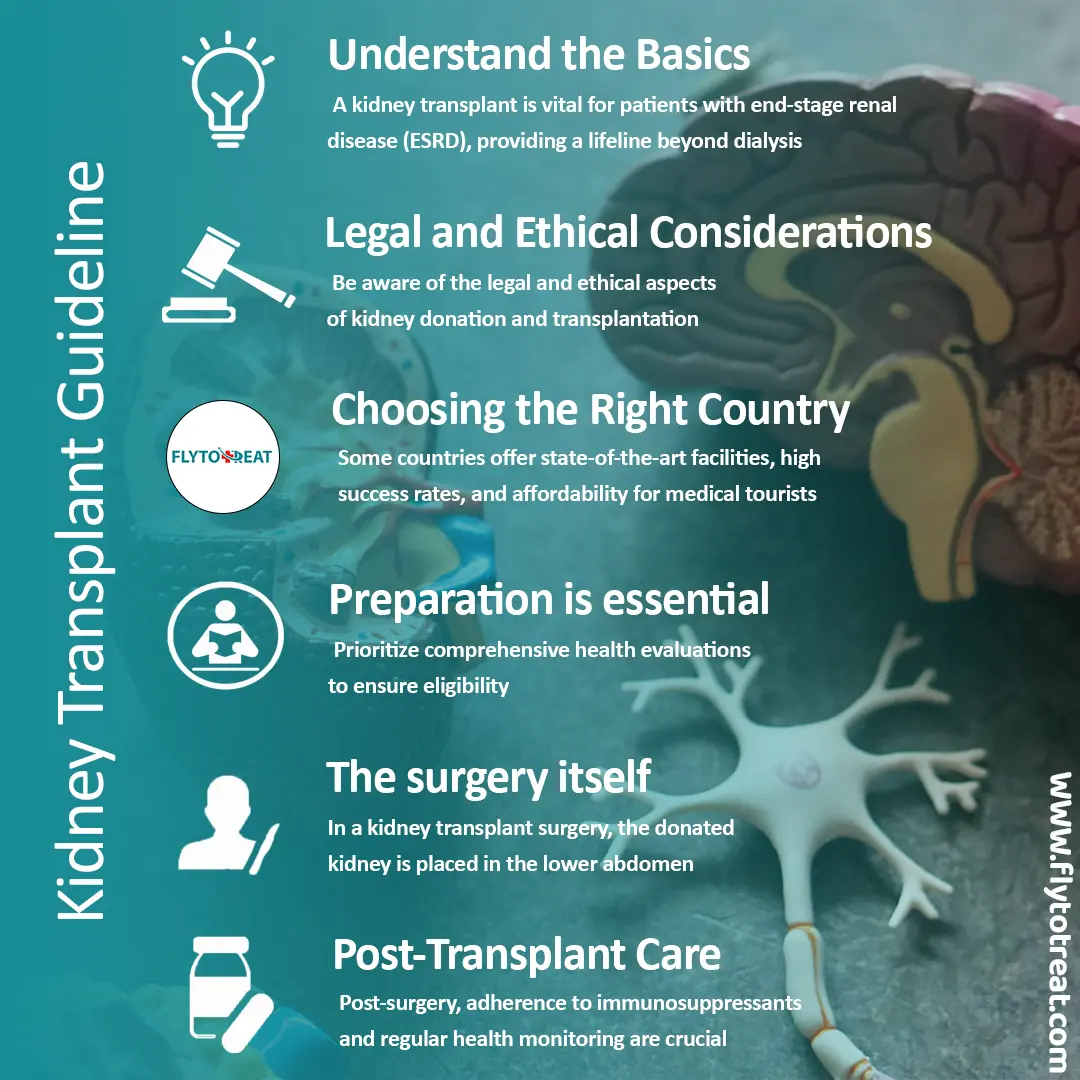
Comprehensive guidelines for a kidney transplant surgery
This guideline covers kidney transplants in-depth, including vital kidney functions, chronic kidney disease stages, and reasons for the transplant. It discusses transplant specifics, financial aspects, life expectancy, kidney rejection management, donation requirements, and risks. Also, it provides insights into post-transplant recovery, ethical issues, the best countries for the transplant, advantages and disadvantages, legal issues, essential medications, recovery timelines, and waiting lists. Here is a breakdown:
• Understand the Basics: A kidney transplant is vital for patients with end-stage renal disease (ESRD), providing a lifeline beyond dialysis. It involves transferring a kidney from a donor, living or deceased, to the recipient.
• Legal and Ethical Considerations: Be aware of the legal and ethical aspects of kidney donation and transplantation, especially regarding donor and recipient compatibility and the avoidance of organ trafficking.
• Choosing the best Country for kidney transplant: Countries like Iran offer state-of-the-art facilities, high success rates, and affordability for medical tourists seeking kidney transplantation.
• Preparation is essential: Prioritize comprehensive health evaluations to ensure eligibility. This includes assessing kidney function, compatibility, and overall physical and mental health.
• The surgery itself: In a kidney transplant surgery, the donated kidney is placed in the lower abdomen. Its blood vessels are connected to those in the lower abdomen and the ureter is connected to the bladder.
• Post-Transplant Care: Post-surgery, adherence to immunosuppressants and regular health monitoring are crucial to prevent kidney rejection and ensure the longevity of the transplant.
What does the kidney do?
Nestled deep within your abdomen, your kidneys are unassuming organs that play a crucial role in maintaining your health and well-being. These bean-shaped wonders are responsible for filtering waste products and excess fluids from your blood, ensuring your body remains clean and balanced.
Each kidney contains over a million tiny filtering units called nephrons. These nephrons are the heart and soul of your kidneys' filtration system. They work tirelessly to purify your blood, removing toxins and waste products while preserving essential nutrients.
The kidneys' filtration function is just one part of their intricate role in maintaining homeostasis, the delicate balance of bodily processes that keeps you healthy. They also regulate blood pressure, produce hormones that control red blood cell production and bone health, and help maintain normal blood pH.
Kidney malfunction stages
Stage 1 CKD: Indicating a normal eGFR of 90 or greater and mild kidney damage, this stage may not manifest noticeable symptoms but could reveal signs such as protein in the urine.
Stage 2 CKD: Characterized by an eGFR between 60 and 89 and mild kidney damage, this stage might not exhibit apparent symptoms but could show signs of kidney damage, including protein in the urine or physical damage.
Stage 3 CKD: With an eGFR ranging from 30 to 59 and mild to moderate kidney damage, this stage reflects compromised kidney function. Symptoms such as fatigue, weakness, or swelling in the hands or feet may emerge.
Stage 4 CKD: Marked by an eGFR between 15 and 29 and moderate to severe kidney damage, this stage signifies a decline in kidney function. Symptoms may include swelling in the extremities and lower back pain, representing the final stage before kidney failure.
Stage 5 CKD: Signifying an eGFR of less than 15 and severe kidney damage, this stage implies imminent or complete kidney failure. Survival necessitates dialysis or a kidney replacement.
Why do people need kidney transplants?
A kidney transplant may be necessary if you're diagnosed with end-stage renal disease (ESRD), a permanent condition characterized by kidney failure often requiring dialysis, a procedure to eliminate toxins and other substances from the blood.
Various kidney conditions can lead to ESRD, including:
• Recurrent urinary infections
• Kidney failure stemming from diabetes or hypertension
• Inherited disorders like polycystic kidney disease
• Glomerulonephritis, characterized by inflammation of the kidney's filtering units
• Hemolytic uremic syndrome, a rare disorder causing kidney failure
• Autoimmune diseases such as lupus
• Obstructions
• Certain congenital kidney defects may also necessitate a kidney transplant.
Additionally, your healthcare provider may recommend a kidney replacement for other reasons.
What are the 3 types of kidney transplants?
As mentioned before, a kidney transplant is a life-saving surgery for people with end-stage kidney disease. There are 3 main donor options to consider:
Deceased Donor Transplant: A kidney transplant from a deceased donor who has recently passed away but has healthy kidneys. This is the most common type of transplant, but wait times can vary.
Living Donor Transplant: A kidney transplant from a living person, donating one of their healthy kidneys. This option offers faster surgery scheduling but requires a compatible donor (often a family member or friend).
Living-Undrelated Donor Transplant: A transplant from a living donor who is not a blood relative but is a compatible match through a national matching program. This option expands the donor pool but may also involve longer wait times.
Each type of kidney transplant has its advantages and considerations. Discuss these options with your doctor to determine the most suitable approach for your situation.
What is a kidney transplant surgery?
Renal transplant, also known as kidney transplant, involves the transfer of a kidney into a patient suffering from end-stage kidney disease (ESRD). This procedure is categorized as either deceased-donor (previously referred to as cadaveric) or living-donor transplantation, depending on the origin of the donor organ. Living-donor kidney transplants are then subdivided into genetically related (living-related) or non-related (living-unrelated) transplants, based on the presence or absence of a biological relationship between the donor and recipient.
During kidney transplant surgery, the new kidney from the donor is placed in the lower belly. The blood vessels of the new kidney are connected to the blood vessels in the lower belly, just above one of the legs. Also, the tube that carries urine from the new kidney to the bladder, called the ureter, is connected to the bladder.
Kidney rejection symptoms
Your body is like a unique fingerprint, consisting of cells, tissues, and organs with a special code inherited from your parents. This code tells your immune system, like a vigilant guard, to recognize what belongs and what doesn't. It fights off invaders like bacteria and viruses and even cleans up old or damaged cells.
But when you receive a kidney transplant, your immune system might see it as foreign and try to attack it. That's called rejection. To prevent this, you'll take special medications called immunosuppressants, like a peace treaty for your body and the new kidney. Taking them regularly is crucial, but sometimes rejection can still happen. This is called a "rejection episode."
During an episode of acute rejection, you might notice one, several, or all of the following symptoms:
• Sensitivity or discomfort around the kidney transplant area
• Generalized body aches
• Swelling in the hands and feet
• Elevated body temperature
• Rapid weight gain
• Higher blood pressure
• Increased blood creatinine levels
• Reduced urine output
Kidney donation requirements
kidney transplant requirements for recipient and donor is most important criteria must consider before any steps of transplant.
Before proceeding with the decision to become a kidney donor, certain basic requirements must be met. Generally, a kidney donor should:
• Be 18 years of age or older
• Be in good physical and mental health
• Have normal kidney function
If you express interest in being a kidney donor, you will undergo medical and psychological evaluations to ensure your overall health and suitability for kidney donation. The transplant center will conduct a series of medical tests to determine compatibility with the recipient and readiness for surgery. Before kidney donation, you will undergo:
• Blood tests
• Tissue typing tests
• Antibody tests
• Pre-surgery health screening
The health of both the donor and the potential recipient is taken into account during the screening process. Certain medical conditions, such as high blood pressure, diabetes, cancer, HIV, hepatitis, or severe infection, may disqualify you from being a kidney donor. Smoking habits may also be considered.
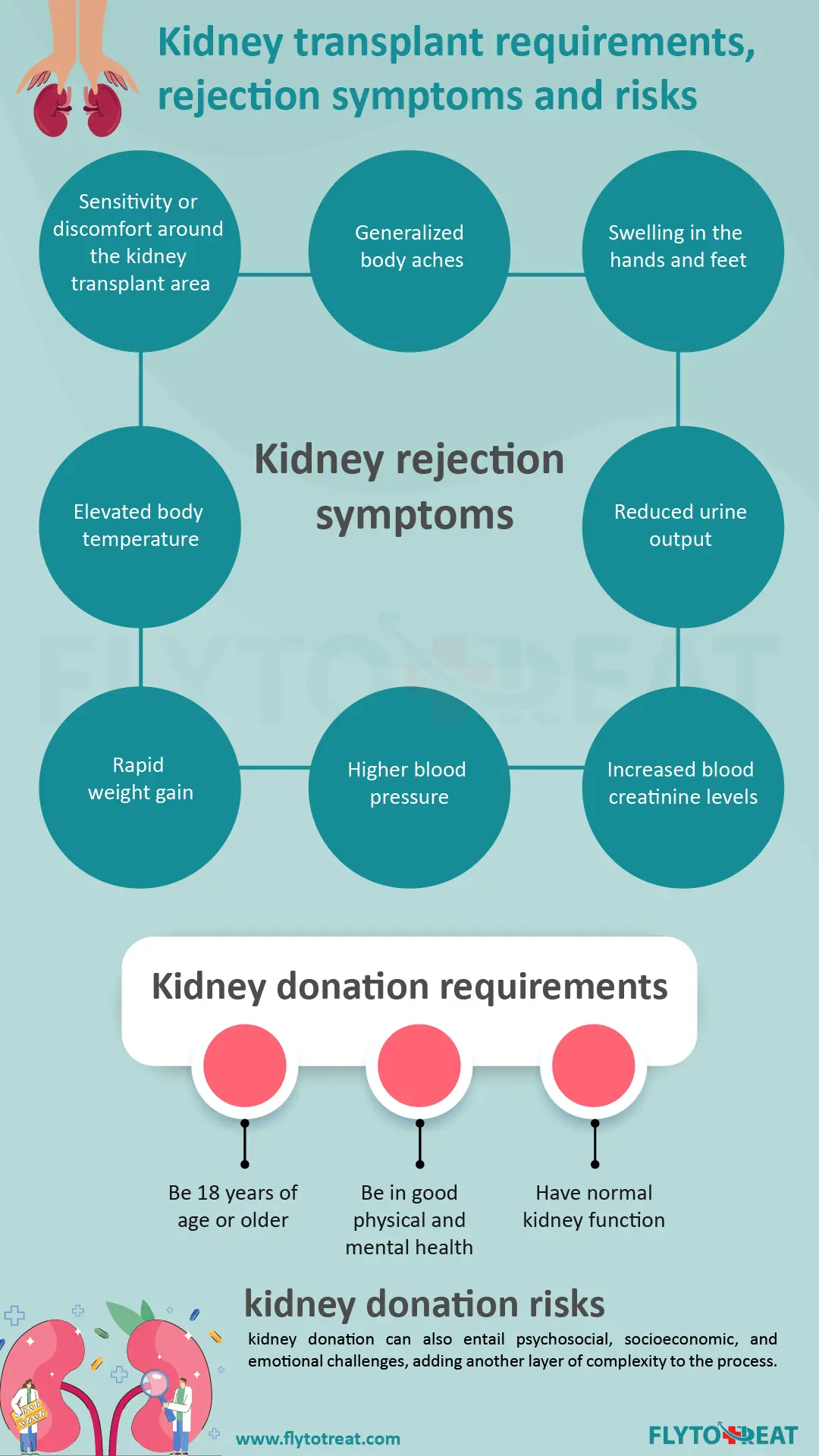
kidney donation risks
Kidney donation is a profound decision that comes with both immediate surgical risks and long-term medical considerations. From potential complications during surgery to the possibility of developing health issues affecting the remaining kidney, donors must carefully weigh the risks and benefits. Moreover, the decision to donate a kidney can also entail psychosocial, socioeconomic, and emotional challenges, adding another layer of complexity to the process. However, with the support of dedicated donor teams, individuals contemplating living donation can navigate these concerns with guidance and assurance.
What happens after a kidney transplant?
Following a kidney replacement, here's what you can expect:
Hospital stay: You'll be in the hospital for a few days, up to a week, while closely monitored for any complications in the dedicated transplant recovery area.
New kidney function: Ideally, your new kidney will start functioning right away, producing urine as your healthy kidneys did. Sometimes, it might take a few days, requiring temporary dialysis until proper function is established.
Recovery and activity: Expect some soreness around the incision as you heal. Most people can return to work and normal activities within 8 weeks. Avoid lifting heavy objects (over 10 pounds) or strenuous exercise (except walking) until your wound heals completely (usually 6 weeks).
Follow-up care: Frequent checkups are crucial post-transplant. This allows doctors to monitor your new kidney's function and prevent rejection.
Intensive monitoring: Initially, you might need weekly blood tests and medication adjustments. If you live far from the transplant center, consider temporary accommodation nearby during this critical phase.
Lifelong medication: Be prepared to take several medications daily for the rest of your life. These primarily include immunosuppressants to prevent rejection and other drugs to minimize post-transplant complications like infections.
Kidney transplant ethical issues
Organ transplantation raises ethical concerns, especially regarding informed consent, which affects donors and recipients. Sources of organs (living, deceased, brain-dead) raise debates like presumed consent, and balancing societal needs with individual autonomy. Developing countries face additional challenges due to socioeconomic and cultural factors. Living donation presents ethical dilemmas like coercion in familial settings and financial motives in non-related donors. Respecting human life and dignity through the "dead donor" rule is crucial, but defining death remains complex. Cultural and religious views add layers to the ethical landscape. Navigating these complexities requires balancing medical progress with ethical principles like autonomy, beneficence, and respect for human dignity.
Best countries for kidney transplant
While seeking a kidney transplant, navigating the varying landscapes across different countries can be complex. Each nation offers unique pros and cons, impacting a crucial decision for patients. Key considerations involve cost, healthcare quality, success rates, and legal frameworks.Countries like India, Turkey, Spain, Thailand, Egypt, South Korea, Israel, Germany, and Mexico all boast strengths in specific areas. However, Iran is a best place for kidney transplant because of its compelling combination of factors.
Firstly, Iranian medical centers consistently report impressive success rates, offering hope and confidence to prospective patients. Secondly, the nation boasts cutting-edge medical infrastructure, ensuring access to advanced technologies and expertise. Finally, compared to many destinations, the cost of transplant surgery in Iran remains highly affordable, making it a viable option for a broader range of patients.
kidney transplant in Iran
Kidney transplants in Iran for foreigners have become one of the most popular options in recent years. This is because the quality of medical services is comparable with that of developed countries, while the costs of residency, livelihood, recreation, and of course, treatment are more affordable than ever for foreigners.
Iran has emerged as a premier destination for kidney replacement procedures, drawing patients from around the globe. Renowned for its top-notch medical facilities, high kidney transplant success rate, and skilled surgeons, Iran boasts an array of transplantation centers, ensuring minimal wait times for patients in need. The country's lenient regulations, requiring only that the donor and recipient share the same nationality, further streamline the process. This ease of access, coupled with the affordability of treatment and living expenses, has made Iran a sought-after destination for medical tourists seeking kidney transplants. The country is the easiest destination to get a kidney transplant.
Among the plethora of transplantation centers, Iran's adept surgeons stand out, renowned for their expertise and commitment to patient care. Fly To Treat, which is a leading medical tourism company, facilitates seamless access to Iran's renowned transplant centers, providing comprehensive services from visa acquisition to post-surgery care.
conclusion
As a conclusion for this comprehensive guideline, kidney transplantation stands as a beacon of hope for individuals grappling with end-stage renal disease (ESRD), offering a pathway to renewed health and vitality beyond the constraints of dialysis. This transformative procedure not only extends patients' lifespans but also significantly enhances their quality of life, freeing them from the burdens of ongoing medical treatment.
However, the journey towards transplantation is not without its complexities. Ethical considerations surrounding organ donation, coupled with the challenges of organ shortages, underscore the need for informed decision-making among potential donors and recipients alike. International collaboration and robust legal frameworks play a pivotal role in navigating these challenges while ensuring the rights of donors and equitable access for all patients in need.
Moving forward, it is imperative to continue advancing research, raising public awareness, and shaping policies to address the persistent obstacles in organ transplantation. By fostering a collaborative approach and prioritizing the well-being of individuals with kidney failure, we can strive towards improved outcomes and a brighter future for all.
Moreover, through platforms like Fly to Treat, patients can access updated technologies, comprehensive support services, and personalized care throughout their transplant journey, ensuring a seamless and successful experience.
MEDICALLY REVIEWED BY: Dr. Ali Bazazi
AUTHOR: FlytoTreat's team of Authors
13 February 2024 - Updated At: 11 December 2024
Related Articles
Comment





