Which country has the easiest kidney transplant rules?
Kidney transplant rules play a pivotal role in determining who can receive this life-changing procedure. With guidance from FlyToTreat, this document outlines the essential contraindications and legal processes involved in kidney transplants across various countries. From managing active infections to navigating international guidelines, these rules ensure that transplants are conducted safely and ethically, offering a new lease on life for those in need. FlyToTreat stands by to offer support and clarity through every step of this complex pathway.
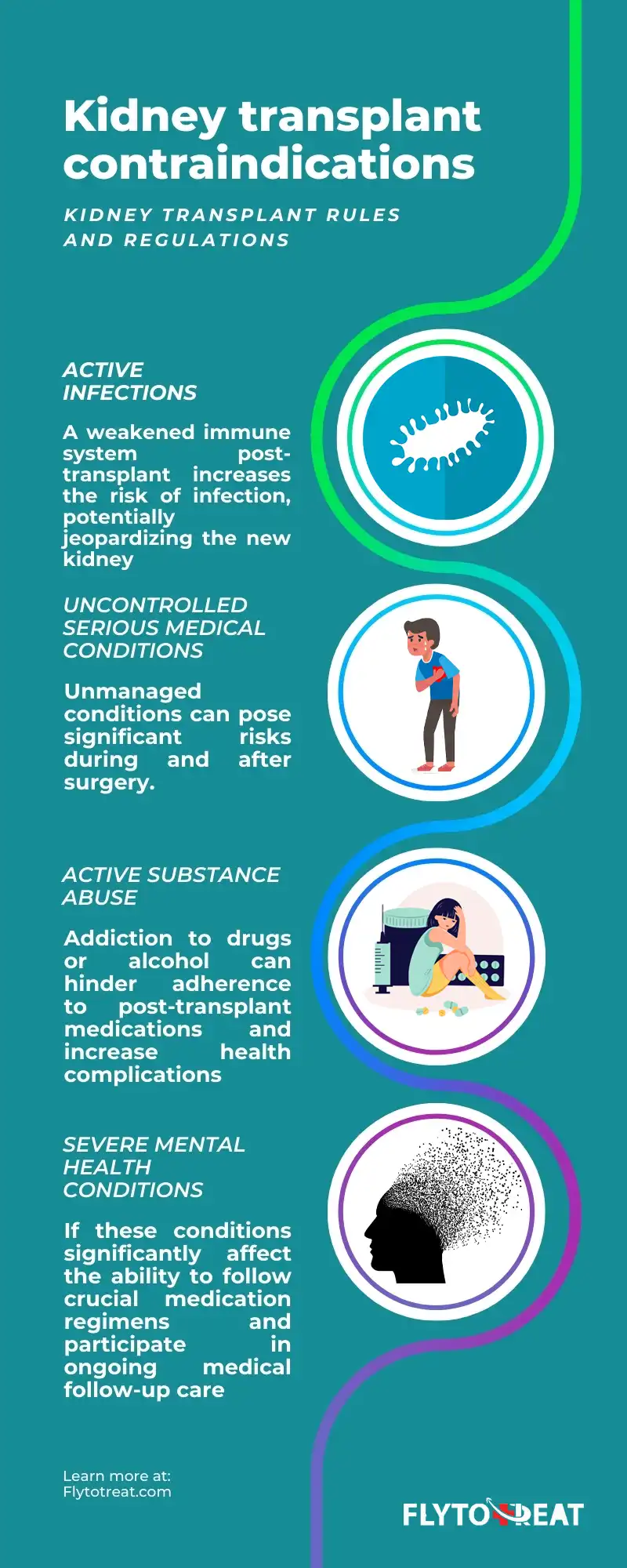
Kidney transplant contraindications
While kidney transplants offer a life-saving option for individuals with end-stage kidney disease, specific kidney transplant rules and regulations determine candidacy. These are based on factors that might adversely impact the success of the surgery or the recipient's long-term health.
According to the studies, critical contraindications include:
• Active infections: A weakened immune system post-transplant increases the risk of infection, potentially jeopardizing the new kidney.
• Uncontrolled serious medical conditions: Unmanaged conditions like severe heart disease, uncontrolled diabetes, or certain cancers can pose significant risks during and after surgery.
• Active substance abuse: Addiction to drugs or alcohol can hinder adherence to post-transplant medications and increase health complications.
• Severe mental health conditions: If these conditions significantly affect the ability to follow crucial medication regimens and participate in ongoing medical follow-up care.
Kidney transplant legal process
Getting a new kidney through a transplant is a big step with many things to consider, both in terms of health and the law. Countries have different kidney transplant rules to ensure things are done fairly and safely.
Many have national laws against buying and selling organs and require donors to agree freely and understand what they're doing (informed consent). These laws often treat living donors who are still alive differently from deceased donors and might also consider the relationship between the two people involved.
On top of these national laws, there are also international guidelines from organizations like the World Health Organization to help make sure organ donation everywhere is done ethically. But unfortunately, in some places, buying and selling organs illegally is still a problem. To stop this, countries must work together and enforce the existing rules.
Even though the legal side of kidney transplants can be complicated and different everywhere, the main goal is the same: to make sure organ donation and transplants are made fairly and safely for everyone involved.
Which country has the easiest kidney transplant rules?
Several countries offer medical services for kidney transplantation for foreigners, and each has its regulations and laws. Often, officials set tight standards to prevent dehumanizing acts of organ trafficking and the growth of black markets. When answering questions like "Which country has the easiest kidney transplant rules?" or best country for kidney transplant. we need to see how the legal system permits the recipients to undergo surgery as immediately as possible.
While many countries have stringent kidney transplant regulations for foreign patients, Iran takes a different approach. Their simplified regulations make it one of the most accessible destinations for those seeking this life-saving treatment globally.
Unlike other countries with burdensome kidney transplant rules limiting access for foreigners, Iran's straightforward legal framework streamlines the process for international patients. This ease of access, the country's reputation for high-quality medical services, and cost-effectiveness attract many individuals needing transplants.
This approach offers a potential answer to the complexities and challenges faced by patients globally who require viable, timely, and efficient medical solutions abroad.
Is kidney transplant legal in Sri Lanka?
Yes, kidney transplants are legal in Sri Lanka, according to the Sri Lanka National Transplant Programme website. However, the country has strict kidney transplant regulations.
In 2015, Sri Lanka banned kidney transplants for foreign nationals due to concerns about organ trafficking. This followed reports of a black market where individuals, primarily from neighboring India, were allegedly paying donors for organs.
Therefore, while legal, kidney transplants in Sri Lanka are restricted to citizens and residents, adhering to the established kidney transplant rules and ethical guidelines set in place to prevent exploitation and ensure fair and ethical practices.
Is kidney transplant legal in Turkey?
Kidney transplants are legal in Turkey and have been performed since the 1970s. The country boasts a well-established healthcare system with experienced transplant teams.
However, strict kidney transplant regulations are in place. These rules govern the process and the participants, ensuring ethical and legal procedures.
Transplants are generally permitted only from living, related donors like close family members or spouses. Additionally, potential donors are thoroughly evaluated to ensure their well-being and ensure the donation is voluntary and free from coercion.
Kidney transplant guidelines in South Africa
In South Africa, the guidelines for kidney transplantation are governed by ethical standards and regulations to ensure the integrity of the organ donation process. The South African Renal Society endorses the Declaration of Istanbul on Organ Trafficking and Transplant Tourism, emphasizing the need for ethical practices in organ transplantation. This declaration advocates against organ trafficking and promotes ethical guidelines for transplantations. The society is actively developing and updating guidelines for kidney transplants, collaborating with governmental and health organizations to enhance the quality and accessibility of renal care. This includes addressing challenges such as dialysis regulation, improving hospital facilities, and advocating for patient and doctor rights. South Africa's commitment to ethical standards and continuous improvement in kidney transplant policies underscores its dedication to patient care and medical ethics in the field of nephrology.
Kidney transplant rules in Pakistan
In Pakistan, kidney transplants are governed by specific regulations outlined in the Transplantation of Human Organs and Tissues Act (2010). These kidney transplant rules aim to ensure ethical practices and prevent exploitation.
Living donors in Pakistan can only be close-blood relatives like parents, siblings, or spouses. Non-related individuals can be donors under exceptional circumstances, with strict evaluations and approval from an authorized committee.
The rules also emphasize that organ donation must be voluntary and free from pressure or financial gain. Additionally, donors and recipients undergo thorough medical assessments to ensure their suitability for the procedure.
Overall, Pakistan's kidney transplant regulations combine ethical considerations with safeguards to protect the well-being of both donors and recipients. Consulting healthcare professionals familiar with these regulations is crucial for anyone considering a kidney transplant in Pakistan.
Kidney transplant law in Bangladesh
In Bangladesh, the Human Organ Transplantation Act of 1999 governs kidney transplantation, allowing organ donation only between living-related donors to combat the illegal organ trade. Amendments in 2018 expanded donor eligibility, including spouse donation, under strict regulatory oversight to ensure ethical practices. This framework prioritizes the ethical procurement of organs, aiming to balance the urgent need for organ transplants with stringent measures against organ trafficking, reflecting a commitment to ethical medical practices and patient safety.
kidney transplant rules in India
Kidney transplant is a life-saving procedure for patients with end-stage renal disease. However, it also involves ethical and legal issues that must be addressed. The Transplantation of Human Organs Act of 1994 is the primary legislation that regulates kidney donation and transplant in India. The Act aims to prevent organ trade commercialization and ensure that donors give informed consent.
According to the Act, kidney donors can be either near relatives or other than close relatives. Near relatives include spouses, parents, children, siblings, grandparents, and grandchildren. Other than immediate relatives include friends, acquaintances, or strangers who donate for love, affection, or other special reasons. However, both types of donors need approval from an Authorization Committee before the transplant. The Committee verifies the identity, relationship, medical fitness, and motivation of the donor and the recipient. The Committee also ensures that there is no payment or coercion involved in the donation.
The Act prescribes various forms and documents that the donor and the recipient must submit to the Committee. These include certificates of residence, family structure, police verification, medical fitness, genetic relationships, etc. The donor and the recipient must also give affidavits stating their consent and reasons for donation. The Act also provides penalties for violation of its provisions.
Rules for kidney transplant in Iran
Iran's kidney transplantation regulations highlight a unique approach, allowing transplants without the necessity for familial connections between donor and recipient, a practice uncommon in many parts of the world. The only kidney transplant policy in Iran is that the donor and the recipient must be of the same nationality. This framework facilitates an efficient process for Iranians and foreigners, notably without waiting lists for international recipients. The "Iranian Model of Renal Transplantation," specifically the Living Unrelated Renal Donation (LURD) system, operational since 1988 under the Ministry of Health's oversight, ensures legal and swift procedures. The success rate of renal transplants in Iran exceeds 95%, attributed to expert surgeons, modern equipment, and rigorous donor assessment, ensuring high-quality kidney donations. Moreover, the cost efficiency of the Iranian model, significantly lower than in many countries, makes it a compelling choice for patients seeking affordable and effective treatment options.

Kidney transplant between siblings (family members)
Sibling compatibility can be a significant advantage when considering a kidney transplant.
Family members, particularly siblings, share a significant portion of their genetic makeup, increasing the likelihood of kidney transplant successful rate. This match compatibility reduces the risk of rejection, a key concern in transplantation.
However, even within families, kidney transplant regulations and ethical considerations exist. Thorough medical evaluations are crucial to ensure the potential donor and recipient are physically and mentally healthy enough to undergo the procedures. Additionally, the decision to donate a kidney must be entirely voluntary and free from pressure or coercion.
Having a sibling as a potential donor can offer hope for those battling kidney disease, but navigating the process requires careful consideration of both medical and ethical aspects.
Conclusion
In conclusion, we provided a comprehensive overview of the complex landscape of kidney transplant regulations and ethical considerations across various countries. We highlighted the significant differences in legal frameworks, donor eligibility criteria, and ethical guidelines implemented to ensure fair and safe organ transplantation practices.
The exploration delved into specific contraindications that can affect an individual's candidacy for a transplant, the legal processes involved in different jurisdictions, and the ongoing global challenge of organ trafficking. The text emphasized the crucial role of ethical standards, informed consent, and international cooperation in promoting responsible organ donation and transplantation. This approach strives to balance addressing the urgent need for organs and upholding rigorous ethical and legal safeguards.
MEDICALLY REVIEWED BY: Dr. Ali Bazazi
AUTHOR: FlytoTreat's team of Authors
02 April 2024 - Updated At: 10 July 2024
Related Articles
Comment




