
What medicine to take after kidney transplant?
Understanding medicine after kidney transplant is crucial for the longevity and effectiveness of the new organ. FlyToTreat offers comprehensive insights into the necessary medications and protocols to ensure a successful post-transplant recovery. This article will cover essential topics such as "kidney transplant medication protocol" and "drugs given after kidney transplant," guiding patients through their post-operative journey.
Kidney Transplant Requirement
A kidney transplant can be life-changing, and it is an excellent alternative to long-term use of dialysis and its devastating side effects. However, kidney transplantation is not for everyone. Here's a glimpse into the vital kidney transplant requirements:
• End-Stage Kidney Disease: Your kidneys must be severely damaged and unable to function adequately on their own. Dialysis, a blood-filtering treatment, is often used before reaching this stage.
• Overall Health: You need to be healthy enough to undergo surgery and tolerate lifelong medication use. Certain medical conditions might make a transplant too risky.
• Blood Type Compatibility: A compatible blood type between you and the donor is and increase kidney transplant success rate crucial to reduce kidney tranplant rejection risks.
• Commitment to Medication: Following a strict medication regimen (usually immunosuppressant drugs) is vital to prevent the body from rejecting the new kidney. This long-term commitment is essential for the success of the transplant.
A transplant team will thoroughly evaluate your health and suitability for surgery. While kidney transplant medications are a necessary part of the process, they require dedication and follow-up to ensure the long-term success of the transplant.
Kidney Transplant Donor Requirements
• Age Requirement: Donors must be over 18 years old to ensure legal capacity and maturity in decision-making.
• Commitment: Donors must demonstrate a steadfast commitment to the donation process, including pre-donation evaluation, surgery, and recovery.
• Physical and Psychological Assessment: Donors undergo thorough assessments to ensure optimal physical and mental health, reducing risks associated with donation.
• Compatibility: Donors' kidney function must be within normal parameters, and blood type compatibility with the recipient is crucial for successful transplantation.
These criteria ensure the safety and efficacy of kidney transplantation from living donors. For more comprehensive information on kidney transplant donor requirements, don’t hesitate to check the link
Medications to Avoid After a Kidney Transplant
While many medications can be helpful, some can be harmful after a kidney transplant. Here's what to avoid:
• Non-steroidal anti-inflammatory Drugs (NSAIDs): These medications, like ibuprofen or aspirin, can damage your kidneys and hinder the function of your new one.
• Over-the-counter (OTC) Medications: Always consult your transplant team before taking any OTC medications, including pain relievers, herbal supplements, or cold remedies. Some ingredients can interact with your kidney transplant medications.
• Specific Antibiotics and Antivirals: Certain medications can affect how your body absorbs your anti-rejection drugs. Your transplant team will prescribe safe alternatives.
Communication is key. Always discuss any medications, including OTC and supplements, with your transplant team before taking them. They can advise you on safe alternatives and ensure your new kidney stays healthy.
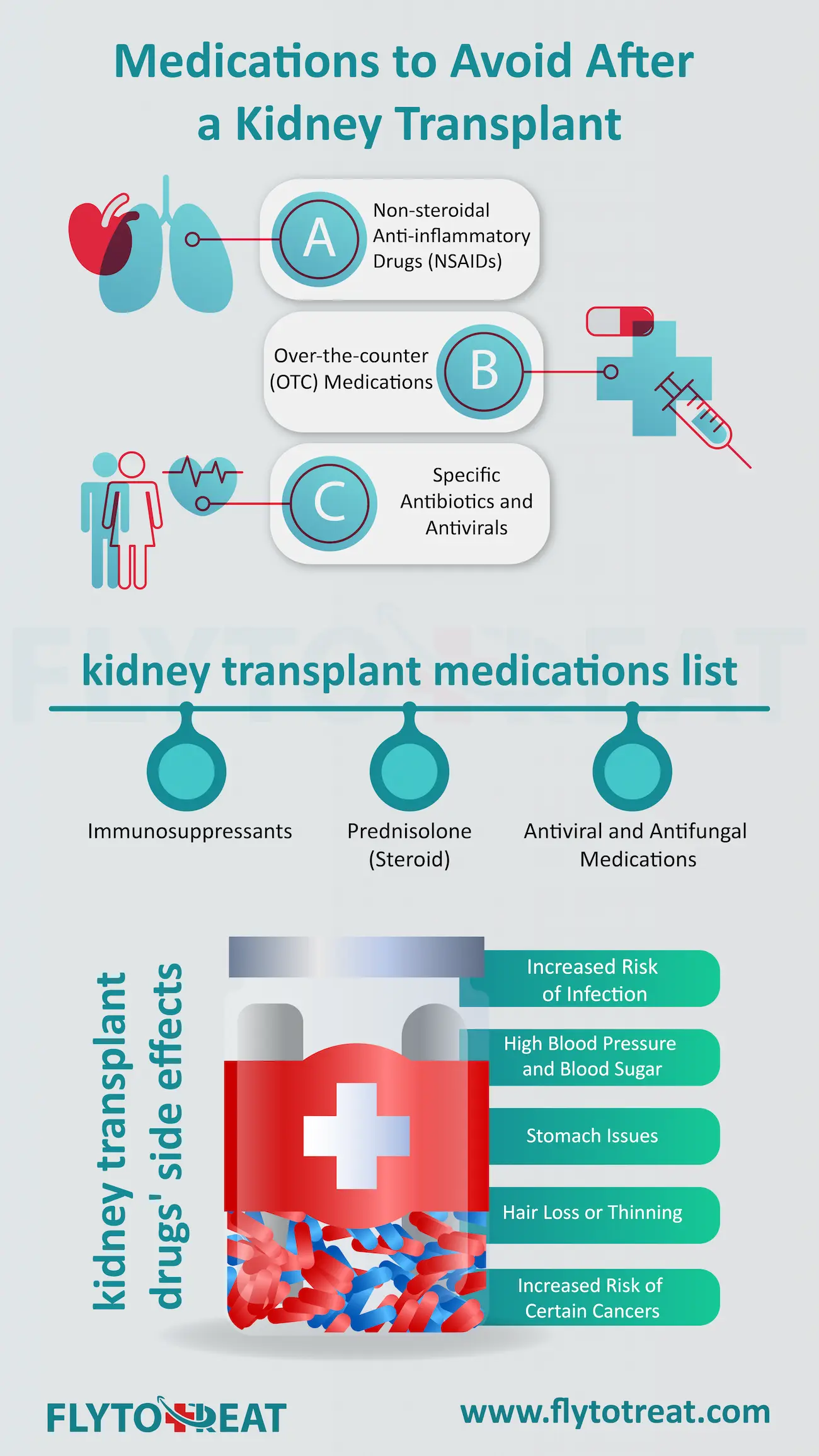
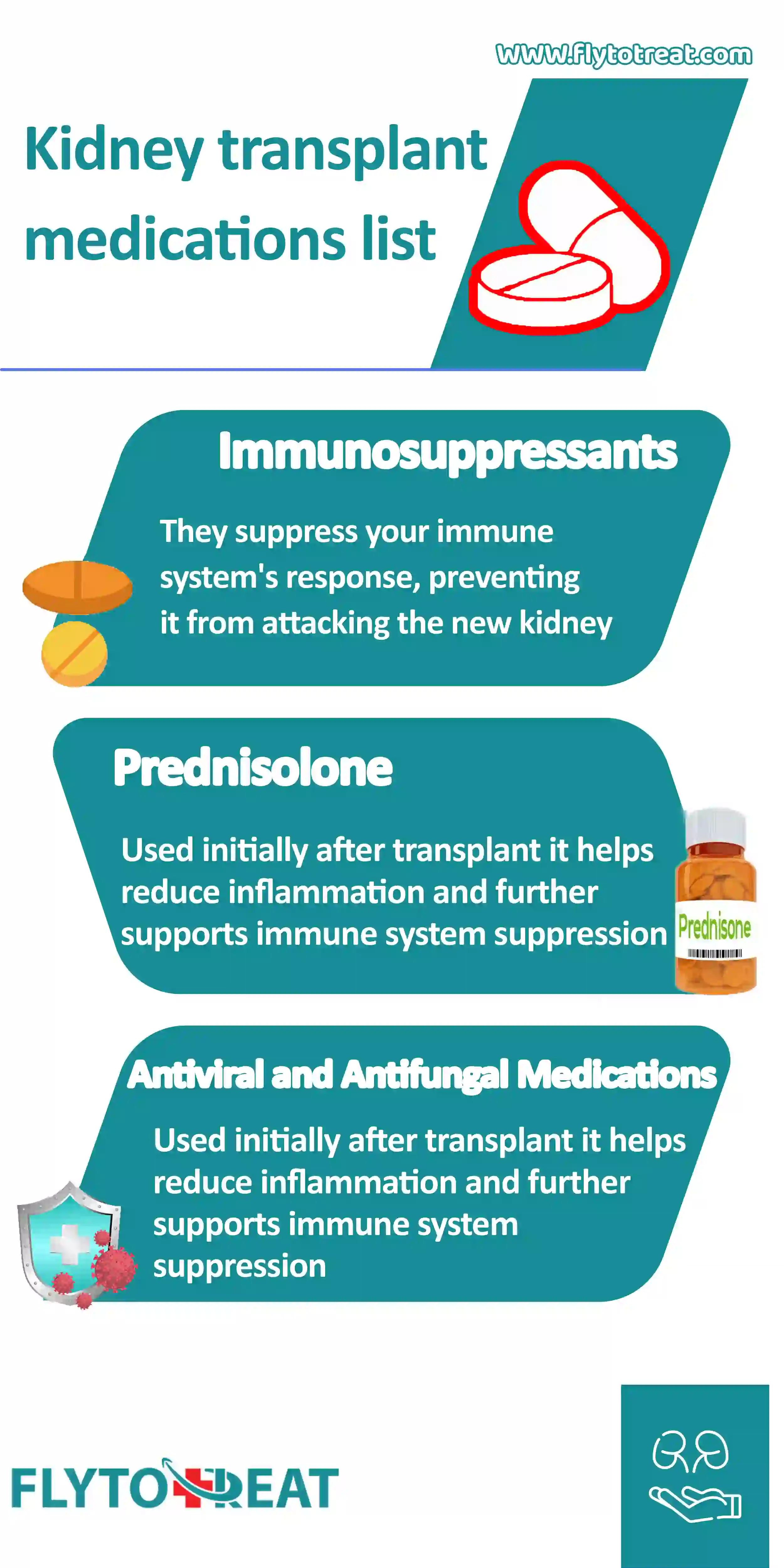
kidney transplant medications list
Following a kidney transplant, you'll take medications to prevent rejection and ensure your new kidney thrives. Here's a peek at some of the common kidney transplant medications:
• Immunosuppressants: These medications are the cornerstone of post-transplant care. They suppress your immune system's response, preventing it from attacking the new kidney as a foreign object. Immunosuppressants or rejection medication for kidney transplants include Tacrolimus, Cyclosporine, Mycophenolate Mofetil, and Azathioprine.
• Prednisolone (Steroid): Often used initially after transplant, Prednisolone helps reduce inflammation and further supports immune system suppression. The dosage is typically reduced over time.
• Antiviral and Antifungal Medications: These medications help prevent infections, which are a greater risk after transplant due to immunosuppression.
This is not an exhaustive list, and the specific medications you take will depend on your individual needs and the transplant team's protocol. Your doctor will determine the renal transplant drugs best suited for you and closely monitor your response to ensure optimal results.
kidney transplant drugs' side effects
While kidney transplant medications are crucial for preventing rejection, they can come with side effects. Here are some to watch for:
• Increased Risk of Infection: Immunosuppressants weaken your immune system, making you more susceptible to infections.
• High Blood Pressure and Blood Sugar: Certain medications can raise blood pressure or blood sugar levels, requiring close monitoring and potential medication adjustments.
• Stomach Issues: Nausea, diarrhea, or vomiting can occur with some medications.
• Hair Loss or Thinning: This is a potential side effect of some renal transplant drugs.
• Increased Risk of Certain Cancers: Immunosuppression can slightly elevate cancer risk. Regular screenings are crucial.
This is not a complete list, and the severity of side effects can vary. Open communication with your transplant team is critical. Discuss any side effects you experience so they can be addressed and your kidney transplant medication regimen can be adjusted if needed. By working together, you can manage side effects and optimize the success of your transplant.
Kidney transplant medication protocol
Kidney transplant medication protocols are not a one-size-fits-all approach. Here's what you need to know:
• Individualized Plan: Your transplant team creates a personalized medication regimen based on your specific needs and risk factors. This considers factors like your immune system, donor compatibility, and overall health.
• Combination Therapy: The protocol typically involves a combination of renal transplant medications, often including immunosuppressants, to prevent rejection. Steroids and antiviral/antifungal medications might also be used.
• Dose Adjustments: The doses of kidney transplant drugs may be adjusted over time as your body adjusts to the new kidney and your risk of rejection changes.
Following your kidney transplant medication protocol precisely as prescribed is crucial for the long-term success of your transplant. Regular check-ups with your transplant team allow them to monitor your progress and adjust your medications as needed.
Can kidney transplant patients take Ozempic?
While Ozempic shows promise for slowing kidney disease progression, information on its use in kidney transplant patients is limited. Studies on Ozempic's safety and efficacy after transplant are ongoing. Kidney transplant medication regimens are personalized. Your doctor considers factors like existing medications and anti-rejection needs. Discuss Ozempic with your transplant team. They can advise on the best course of action for your specific situation, considering both potential benefits and interactions with your current renal transplant medications.
Can kidney transplant patients take b12?
Yes, kidney transplant patients can take vitamin B12, but consult your doctor first. Studies suggest a higher prevalence of B12 deficiency in transplant patients, possibly due to certain medications or dietary factors. Your doctor can check your B12 levels and recommend supplementation if needed.
Allergy medicine for kidney transplant patients
Kidney transplant patients and allergy sufferers need careful consideration when choosing medication. Here's why:
• Immunosuppressant Interaction: Certain allergy medications, especially immunosuppressants, can interact with renal transplant medications, affecting the effectiveness of either medication.
• Safer Options Available: Many allergy medications are safe for transplant patients, but it's crucial to consult your doctor. They can recommend safe alternatives like non-drowsy antihistamines.
Never take over-the-counter allergy medications without consulting your transplant team. They can advise on the safest options to manage your allergies while keeping your transplant healthy.
What can kidney transplant patients eat?
Following a kidney transplant, a healthy diet is crucial for optimal health and long-term success. Here's a glimpse into what kidney transplant patients can eat:
• Fruits and Vegetables: Fill your plate with a colourful variety of fruits and vegetables. They provide essential vitamins, minerals, and fibre to support your overall health.
• Lean Protein Sources: Include lean protein sources like fish, poultry, beans, and lentils in your diet. These are essential for building and maintaining muscle mass.
• Limit Processed Foods, Salt, and Sugar: Processed foods, added salt and sugary drinks can put a strain on your new kidney. It is advisable to choose fresh, whole foods whenever they are available.
• Maintain Healthy Portion Sizes: While enjoying a variety of foods, be mindful of portion sizes. This helps manage weight and blood pressure, both critical factors for kidney health.
Your transplant team, including a registered dietitian, can create a personalized meal plan to address your specific needs and preferences. They can also offer guidance on managing potassium, phosphorus, and fluid intake, which may be necessary for your kidney health.
Conclusion
To wrap up, the medicine regimen after a kidney transplant plays a pivotal role in the success and health of the transplant recipient. FlyToTreat provides essential information and support for navigating the complexities of medications such as immunosuppressants and antivirals and the adjustments needed over time. By understanding the various aspects of post-transplant care, including potential side effects and the importance of adherence to prescribed treatments, patients can achieve the best possible outcomes and lead a healthy post-transplant life.
MEDICALLY REVIEWED BY: Dr. Ali Bazazi
AUTHOR: FlytoTreat's team of Authors
12 May 2024 - Updated At: 26 October 2024
Related Articles
Comment





